Peripheral Artery Disease/Intervention
Peripheral Arterial Disease (PAD, or sometimes referred to as Peripheral Vascular Disease or PVD) refers to a buildup of plaque on the inner lining of the arterial walls (atherosclerosis). These deposits can cause a narrowing of the arteries, and therefore decrease the blood flow through the arteries of the legs or arms. This can cause ischemia, or lack of blood supply and oxygenation to the muscles and tissue, most often in the legs and/or feet.
It is estimated that approximately 10 million people in the United States have PAD. Many people with PAD are without symptoms. The classic symptoms of PAD typically begin with pain, tightness, early fatigue or a cramp-like feeling in the legs/calves/buttocks during activity or exertion. When the person is at rest or stops the activity, this pain subsides. This is called “intermittent claudication”. Because leg pain can be due to many different causes, these symptoms are often dismissed by patients as being due to arthritis, old injury, or other causes. If the leg pain is due to PAD and continues to go undiagnosed, this allows the disease to progress and can result in more serious consequences of PAD, such as leg pain at rest, gangrene, or limb loss.
PAD can be easily diagnosed by a simple, noninvasive test called the ankle-brachial index or ABI. This test measures the blood pressure in the arm and the legs and looks for any significant difference. An abnormal study can diagnose PAD as a likely cause of leg pain. Additionally, because PAD can be an early marker for more extensive vascular disease (such as coronary artery disease and carotid artery disease), an abnormal ABI can identify people at higher risk for heart attack and stroke. Finally, screening for PAD with an ABI allows patients with PAD to be treated earlier in the disease process, reducing the risk of the long-term consequences of PAD.
Risk factors for PAD include: hypertension (high blood pressure), diabetes, high cholesterol, smoking, and being physically inactive.
If diagnosed with significant PAD the vascular anatomy must be evaluated. This is typically done with one or more types of vascular imaging, including ultrasound, CT scan, or MRI to specifically look at the circulation. If there is significant obstruction of the arteries to the legs certain interventions may be warranted to help improve the circulation and reduce lifestyle-limiting symptoms. In certain situations an angiogram (also known as an arteriogram) may be necessary.
An angiogram is a procedure performed by an interventional radiologist in which a catheter is inserted through the artery in the groin and contrast is injected into the arteries in the legs. This allows the physician to visualize the arteries and see the areas that are partially or completely blocked. If an area of the vessel is blocked and requires treatment there are several options for nonsurgical intervention, including balloon angioplasty, atherectomy (plaque removal) and stent placement. These procedures entail placing a balloon and/or stent (a small, metal mesh tube) into the artery at the narrowed area and expanding it in order to increase the diameter of the vessel and improve blood flow and long-term patency. There may be the need for placement of more than one stent depending on the extent of the PAD. Sometimes devices that remove plaque are used depending on the artery that is involved. On occasion the best treatment may be a surgical approach. If this is the case a referral to a cardiovascular surgeon may be given. Otherwise a minimally invasive approach is usually favored by most patients.
Most of these cases are outpatient procedures done with local anesthetic and light sedation, either at our outpatient center or at the hospital. This will be decided by your VIP physician after discussing the options with you.
Preparing for your Peripheral Artery Angioplasty/Stenting:
- A representative will call you prior to your procedure to review instructions and complete registration.
- You will need to arrange for a driver to take you home.
PRE-OP:
- You may need further imaging such as an MRA or a CTA prior to the procedure.
- Do not eat or drink anything for 12 hours prior to your procedure.
- Make sure to let your doctor know if you are on any blood thinners, including Coumadin (Warfarin), Heparin, Lovenox, Plavix or over-the-counter medications such as Aspirin.
INTRA-OP:
- The procedure itself is not painful, however light sedation medications will be administered through an IV in order to prevent any discomfort.
- The entire procedure is done sterilely, so you will have a large drape placed over your body in order to maintain sterility.
- After application of local anesthesia a catheter (tube) will be placed into the large artery in the groin. (You will not be able to feel the catheters as they move through the arteries)
- Before placing the stent an arteriogram (injection of contrast dye into the arteries) is performed to provide a roadmap of the blood vessels.
- Angioplasty (ballooning) of the vessel may be performed prior to and during placement of the stent.
- Once the stent/stents is/are deployed the catheter will be removed from the groin and a dry sterile dressing will be applied to the area.
- The procedure typically takes between 2-3 hours to complete, however it may last longer in some circumstances.
POST-OP:
- After the procedure you will need to lie flat for approximately 3-4 hours.
- You may begin to eat a regular diet once you are able to tolerate oral intake.
- Patients are typically discharged home after 4-6 hours and may resume normal activities after 24-48 hours.
- When you return home you may be instructed to take certain blood thinning medications in order to prevent clots from forming.
If you develop fever or severe pain contact our office at 352-333-7847 (7VIP) or call your referring physician. After hours or on weekends go to the nearest emergency room or call North Florida Regional Medical Center at 352-333-4000 and ask for the Interventional Radiologist on call.
Abdominal Aortic Aneurysm Treatment
The aorta is the largest artery in the body, carrying blood through the chest and abdomen, supplying several vital organs along the way. Below the navel the aorta splits into two branches diving deep into the pelvis. These smaller vessels, called the iliac arteries, carry blood through important structures in the pelvis and then continue on into each leg.
 Normally the aorta measures approximately 1 inch (2.5 centimeters) in diameter. A weakness in the wall of the abdominal aorta can develop and under the pressure of flowing blood can form a bulge called an abdominal aortic aneurysm (AAA). Nearly 200,000 people in the United States are diagnosed annually with AAA.
Normally the aorta measures approximately 1 inch (2.5 centimeters) in diameter. A weakness in the wall of the abdominal aorta can develop and under the pressure of flowing blood can form a bulge called an abdominal aortic aneurysm (AAA). Nearly 200,000 people in the United States are diagnosed annually with AAA.
Abdominal aortic aneurysms are often without symptoms and in fact are often discovered incidentally. The most severe and devastating symptom associated with AAA is rupture of the aneurysm, which can result in severe bleeding or even death.
A clot that may form within the aneurysm can sometimes break off and float downstream into smaller arteries in the legs causing an obstruction or in more severe cases loss of the affected limb.
While the exact cause of AAA is unknown, it is most likely to be the result of an inflammation of the aorta, perhaps in combination with certain risk factors, such as hypertension and smoking. Family history may also play a role in the diagnosis of AAA. Men are more commonly affected than women.
Symptoms of AAA
While many people are without symptoms of AAA the most common symptom reported is a “pulsing” sensation in the abdomen. More concerning symptoms in patients with a known AAA are the sudden onset of abdominal and/or lower back pain and the sudden onset of a cold foot or discoloration of the foot/toes, signaling a clot or debris that has broken loose. AAA rupture can lead to the sudden onset of weakness and dizziness associated with abdominal/back pain and is a true medical emergency.
Treatment of AAA
Treatment of AAA is related to size of the aneurysm and a patient’s anatomy. The following list includes treatment options for AAA:
- Watchful waiting is the periodic followup of AAA at regular intervals to determine if it is changing or enlarging. This is typically recommended for “smaller” aneurysms that have not reached the size that dictates intervention; Typically AAAs <5.0cm are observed every 6 months with follow-up ultrasound or CT scans. In certain circumstances aneurysms less than 5.0cm are treated with either approach, such as symptomatic AAA (see section on AAA symptoms) or AAA that may be enlarging rapidly.
- Endovascular aneurysm repair (EVAR) is a less invasive approach to aneurysm repair by interventional radiologists involving the placement of a stent with a graft material attached to it (called a “stent-graft” or “endograft”). This approach is usually done with one or two smaller incisions in the leg, threading the device through the blood vessels into the aorta. This technique is like fixing the aneurysm “from the inside out.” Patients usually spend 2 days or less in the hospital and resume usual activities sooner than with open surgical repair. While there is usually an easier initial recovery with EVAR there is more structured followup with imaging studies like CT scans and occasionally a secondary minor procedure may need to be done to ensure the endograft is working appropriately. Since this procedure is very dependent on anatomy not all AAA patients may be candidates for EVAR.
- Open surgical repair of the aneurysm is typically performed by a cardiovascular surgeon and involves a large abdominal incision with a synthetic flexible tube (called a “graft”) being sewn into the aorta, replacing the aneurysm. This approach typically involves a hospital stay of 4-7 days and usually several weeks for a full recovery. Open repair is less dependent on patient anatomy and therefore most patients are candidates for open surgical repair. In addition, the usual follow-up is less involved than with EVAR.
VIP physicians will discuss all treatment options and make recommendations regarding the best possible approach to your AAA. Depending on which treatment option is recommended the preparation for AAA arterial disorder will vary. Any pre-op discussion will be presented at the time your procedure is scheduled.
If you develop fever or severe pain contact our office at 352-333-7847 (7VIP) or call your referring physician. After hours or on weekends, go to the nearest emergency room or call North Florida Regional Medical Center at 352-333-4000 and ask for the Interventional Radiologist on call.
Carotid Artery Intervention
The Carotid Arteries are the two major arteries in the body that provide blood flow to the brain. The pulse of these arteries can be felt on both sides of the neck and they are vital for delivering oxygen to the brain.
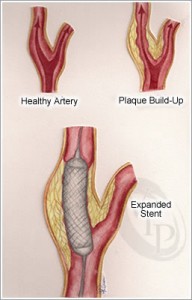 Carotid Stenosis refers to a narrowing of the inner wall of the artery. This usually occurs due to a buildup of plaque, commonly referred to as atherosclerosis. This can cause the inner wall of the artery to become smaller in diameter, thereby decreasing the amount of blood that can flow to the brain.
Carotid Stenosis refers to a narrowing of the inner wall of the artery. This usually occurs due to a buildup of plaque, commonly referred to as atherosclerosis. This can cause the inner wall of the artery to become smaller in diameter, thereby decreasing the amount of blood that can flow to the brain.
If the flow becomes completely blocked or if a piece of plaque breaks loose, a transient ischemic attack (TIA) or an ischemic stroke may occur.
Transient ischemic attacks (TIAs) or “mini-strokes” are episodes of stroke-like symptoms that last less than 24 hours. This may involve slurred speech, facial droop, loss of sensation, or weakness in a limb or on one side of the body. TIAs may be a warning sign and patients with a history of TIA are at increased risk for a stroke, which may cause brain damage and/or death.
Your doctor may detect carotid stenosis when listening with a stethoscope over the artery. If a carotid bruit (abnormal sound) is heard your physician may refer you for a Doppler ultrasound. SEE CAROTID DUPLEX. If carotid stenosis is suspected treatment may be required to help reduce the risk of future stroke. Sometimes a surgical procedure called endarterectomy can be performed, however it has been shown that not all patients are good surgical candidates and some patients may benefit from a less invasive approach.
The minimally invasive treatment for carotid stenosis is Carotid Artery Angioplasty and Stenting. This is a procedure in which a balloon and stent (a small metal tube) are inserted through the artery in the groin and directed up into the carotid artery. The catheter is positioned within the narrowed area and a balloon is expanded in order to increase the diameter of the vessel to improve blood flow. A stent is usually left in place in order to maintain patency of the vessel long term.
Preparing for Carotid Artery Angioplasty/Stenting:
- A representative will call you prior to your procedure to review instructions and complete registration.
- You will need to arrange for a driver to take you home.
PRE-OP:
- You may need further imaging such as an MRA or a CTA prior to the procedure.
- Do not eat or drink anything for 12 hours prior to your procedure.
- Make sure to let your doctor know if you are on any blood thinners, including Coumadin (Warfarin), Heparin, Lovenox, Plavix or over-the-counter medications such as Aspirin.
INTRA-OP:
- The procedure itself is not painful, however light sedation medications will be administered through an IV in order to prevent any discomfort
- The entire procedure is done sterilely so you will have a large drape placed over your body in order to maintain sterility.
- After application of local anesthesia a catheter (tube) will be placed into the large artery in the groin. This catheter will be advanced all the way up to the carotid arteries. (You will not be able to feel the catheters as they move through the arteries)
- Before placing the stent an arteriogram (injection of contrast dye into the arteries) is performed to provide a roadmap of the blood vessels.
- A filter or basket will then be inserted beyond the carotid artery in order to prevent pieces of plaque or clots from breaking away and causing stroke.
- Angioplasty (ballooning) of the vessel may be performed prior to and during placement of the stent.
- Once the stent is deployed the catheter will be removed from the groin and a dry, sterile dressing will be applied to the area.
- The procedure typically takes between 1-2 hours to complete, however it may last longer in some circumstances.
POST-OP:
- Your procedure will require an overnight hospital stay for observation.
- You may begin to eat a regular diet once you are able to tolerate oral intake.
- Patients are typically discharged home after 1-2 nights in the hospital, and a follow up appointment will be scheduled at that time.
- When you return home you will be instructed to take certain blood thinning medications in order to prevent clots from forming within the new carotid stent.
If you develop fever or severe pain contact our office at 352-333-7847 (7VIP) or call your referring physician. After hours or on weekends, go to the nearest emergency room or call North Florida Regional Medical Center at 352-333-4000 and ask for the Interventional Radiologist on call.
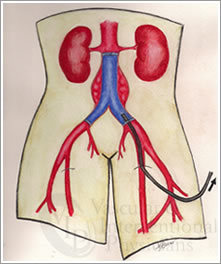
Renal Artery Interventions
The renal arteries are the blood vessels that supply blood to the kidneys. Renal artery stenosis is the term used to refer to a narrowing of the renal artery. This is typically caused by either atherosclerosis (a buildup of plaque) or Fibromuscular Dysplasia (a disease in which the cells in the walls of the arteries undergo abnormal growth which can result in narrowing of the vessels). Renal artery stenosis can be detrimental to the health of your kidneys and may cause uncontrolled hypertension (high blood pressure) as well as kidney failure if left untreated.
In certain patients treatment beyond medication adjustment may be necessary to help restore better blood flow to the kidneys with the goal being to preserve kidney function and better control blood pressure. The main interventional treatment for significant renal artery stenosis is renal artery angioplasty/stent placement.
Angioplasty or stent placement
Angioplasty and stenting is a procedure typically performed on an outpatient basis in which a balloon and/or stent (a small metal tube) is inserted through the artery in the groin into the renal artery. The balloon is positioned within the narrowed area and expanded in order to increase the diameter of the vessel to improve blood flow. A stent is usually left in place in order to maintain patency of the vessel long term.
Preparing for Renal Artery Angioplasty/Stenting:
- A representative will call you prior to your procedure to review instructions and complete registration.
- You will need to arrange for a driver to take you home.
PRE-OP:
- You may need further imaging such as an MRA or a CTA prior to the procedure.
- Do not eat or drink anything for 12 hours prior to your procedure.
- Make sure to let your doctor know if you are on any blood thinners, including Coumadin (Warfarin), Heparin, Lovenox, Plavix or over-the-counter medications such as Aspirin.
INTRA-OP:
- The procedure itself is not painful, however light sedation medications will be administered through an IV in order to prevent any discomfort.
- The entire procedure is done sterilely so you will have a large drape placed over your body in order to maintain sterility.
- After application of local anesthesia a catheter (tube) will be placed into the large artery in the groin. This catheter will be advanced up to the level of the renal arteries. (You will not be able to feel the catheters as they move through the arteries).
- Before placing the stent an arteriogram (injection of contrast dye into the arteries) is performed to provide a roadmap of the blood vessels.
- Angioplasty (ballooning) of the vessel may be performed prior to and during placement of the stent.
- Once the stent is deployed the catheter will be removed from the groin and a dry, sterile dressing will be applied to the area.
- The procedure typically takes between 1-2 hours to complete, however it may take longer in some circumstances.
POST-OP:
- After the procedure you will need to lie flat for approximately 3-4 hours.
- You may begin to eat a regular diet once you are able to tolerate oral intake.
- Patients are typically discharged home after 4-6 hours, and may resume normal activities after 24-48 hours.
- When you return home, you may be instructed to take certain blood thinning medications in order to prevent clots from forming within the new renal stent.
If you develop fever or severe pain contact our office at 352-333-7847 (7VIP) or call your referring physician. After hours or on weekends, go to the nearest emergency room or call North Florida Regional Medical Center at 352-333-4000 and ask for the Interventional Radiologist on call.

Pingback: Peripheral Arterial Disease (PAD): America’s Silent Killer — Risk Factors, Symptoms & Treatment Options | Vascular & Interventional Physicians